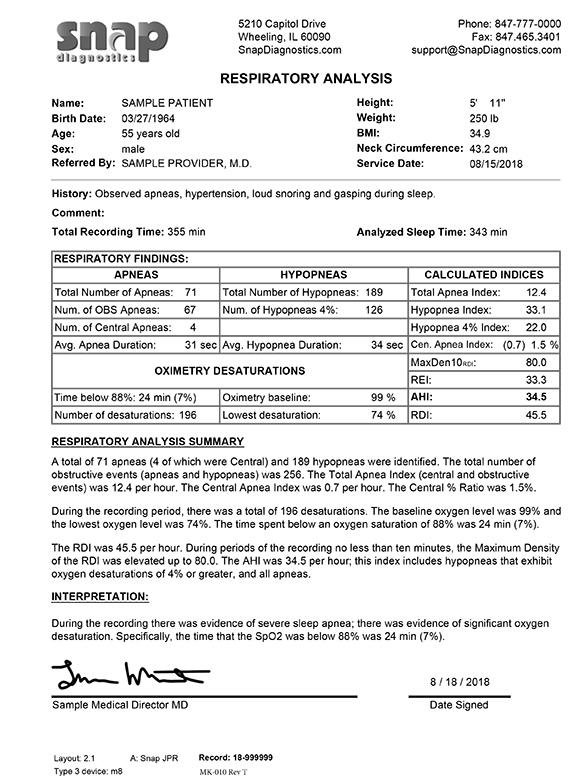
Several studies have linked sleep apnea with neurodegenerative diseases, including Alzheimer’s disease and other dementias. A new study reveals important insights into how sleep apnea may impact the brain in older adults. The study, published in Neurology, found that individuals who have severe sleep apnea and spend less time in deep sleep have increased abnormalities in the white matter of the brain, which may contribute to cognitive decline and disease.
What to Look For:
The most common symptoms of sleep apnea include snoring, gasping, or choking during sleep, morning headaches, and daytime sleepiness. Risk factors associated with sleep apnea include high body mass index (BMI), obesity, older age (>40 years old), and certain anatomical features such as enlarged tonsils or upper airway abnormalities. Use of tobacco, alcohol, and certain sedative and pain medications may increase apnea severity.
Sleep apnea is a common comorbidity in patients with heart disease, stroke, high blood pressure, GI reflux disease, high cholesterol, and type II diabetes.

Recent Comments